ooof
Stories about operable pancreatic cancer
These stories are from people who could have surgery to remove their cancer.
Mark D
Mark was 52 when he was diagnosed with pancreatic cancer. Following successful Whipple’s surgery and chemotherapy he’s back to work and enjoying life.

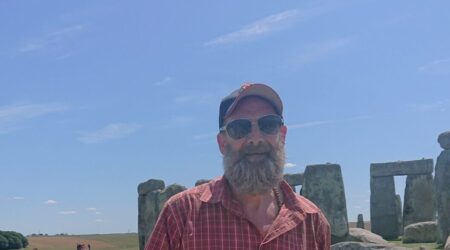
Steve C
Steve, 60, found out he had stage 2 pancreatic cancer by chance in 2023. He reflects on the care and support he has had, the symptoms and side effects of treatment, and the emotional impact on him and his family.

Coral
Coral was diagnosed in 2020 with pancreatic cancer, she was 76 years old. She had a Whipple's procedure but wasn't well enough for chemotherapy. Coral shares her story.

Mary
Mary, 67, was walking home from work in October 2020 when she was struck with extreme tiredness. Within two days, she was given a diagnosis of pancreatic cancer and told she had been diagnosed early enough for surgery.

Pippa
Pippa was diagnosed with a pancreatic cyst in 2010. It was monitored for many years. When changes were spotted, Pippa had surgery and is now recovering well.

Amanda
Amanda was 51 when she was diagnosed with stage 2 pancreatic cancer. She had surgery and chemotherapy and is now having more chemotherapy following a recurrence of the cancer.

Nicola
Nicola had a few weeks of bloating, followed by pale, oily stools and weight loss. She was diagnosed with stage 3 pancreatic cancer. After chemotherapy, Nicola was able to have surgery to remove the cancer. Nicola shares her 'roller coaster' year from diagnosis through treatment on to recovery.

Andrew
Andrew had an abnormal blood test during a routine health screen and later developed jaundice. He had a stent put into his bile duct and a few weeks later had a Whipple's procedure. Andrew shares his experience of diagnosis, treatment and recovery and his message of hope.

Elma
Elma was 69 when she was diagnosed with borderline operable pancreatic cancer, after feeling pain in her stomach. She had surgery and chemotherapy, and five years later, she has been given the all-clear.

Clive
Clive was diagnosed with pancreatic cancer after his daughter noticed he had symptoms of jaundice. He was able to have the cancer removed by a Whipple’s procedure. Clive is recovering well and shares his story to help others who are being diagnosed.

Trevor G
Trevor was 61 when he was diagnosed with cancer in the head of the pancreas. He reflects on the emotional impact of his diagnosis and treatments, and how the support he has had from his wife is helping him through this.

Robert
Robert went to his GP suffering from nausea and was quickly diagnosed with pancreatic cancer, aged 59. He talks about getting treatment and taking part in a clinical trial.