Feeling and being sick at the end of life
In the last few months of life, pancreatic cancer and its treatment can make you feel and be sick.
Read about other symptoms at the end of life
- Pain towards the end of life
- Fatigue at the end of life
- Diet and digestion at the end of life
- Weight loss and reduced appetite towards the end of life
- Feeling and being sick at the end of life
- Stomach emptying slowly towards end of life
- Bowel problems towards the end of life
- Swelling (ascites and oedema)
- Jaundice in the last few months
- Bedsores towards the end of life
- Anxiety and depression towards the end of life
Feeing and being sick can be unpleasant and distressing. It may also mean that you aren’t properly absorbing the medicines you take, such as pain relief.
How is sickness managed?
Speak to your doctor or nurse if you are being sick. They will work out what is causing your sickness, and give you treatment. They may give you anti-sickness medicines. These may be tablets, liquids, or injections. You can also have some anti-sickness medicines through a syringe driver.
If you have been vomiting for a day or more, contact your GP, district nurse, or your GP out of hours service. If you are being sick a lot, there is a risk that you could become dehydrated (where your body loses more water than it takes in).
What causes sickness?
Feeling and being sick in the last few months of life can be caused by:
- cancer blocking the duodenum
- the stomach not emptying, or emptying slowly
- jaundice, when the liver not working properly
- constipation (when you find it hard to poo)
- a thrush infection in your mouth or throat
- some medicines
- anxiety.
Blocked duodenum at the end of life
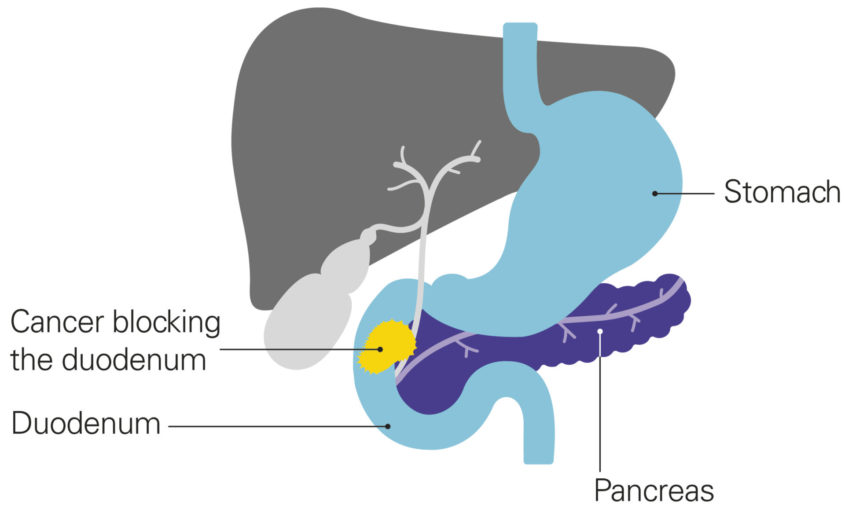
If the cancer blocks the duodenum (the first part of the small intestine), this can cause sickness and make you feel full. This is because food can’t flow out of the stomach.
You may find you are sick more in the evenings or at night, and you may vomit large amounts. You may feel better for a while afterwards but then start to feel sick again. If the duodenum is blocked, you may also lose your appetite and lose weight. It can also cause pain, cramping and bloating in the tummy area.
Diagram showing the cancer blocking the duodenum
A duodenal stent to treat a blocked duodenum
If you have a blocked duodenum, you may be able to have a hollow tube called a duodenal stent put in. This will open the part of the duodenum that is blocked so that food can pass through. This should stop you feeling sick and you should find it easier to eat.
Sometimes stents can become blocked. To stop this happening, try having small meals often, and have soft foods like porridge, minced meat and mashed potato. If the stent does get blocked, it can make you feel sick again, and the stent may need to be replaced. Read more about diet and a duodenal stent.
A duodenal stent won’t be suitable for everyone. You will need to be fit enough to have a sedative (to make you sleepy) to have the procedure.
If you can’t have a duodenal stent
If a stent isn’t suitable for you, your doctor will give you medicine to manage the sickness as well as any other symptoms, such as pain.
Some people may be able to have their stomach drained to stop them being sick. This may be done with a nasogastric tube, which is a tube that passes up your nose and down into your stomach. Or occasionally a tube called a venting gastrostomy tube can be put into the stomach through the skin. A venting gastrostomy tube won’t be suitable for everyone, and may not be used that often.
Questions about sickness?
If you feel or are sick, speak to your doctor or nurse.
You can also speak to our specialist nurses on our free Support Line with questions about sickness.

Read our booklet about end of life care
To read more about feeling and being sick at the end of life, download our booklet, Pancreatic cancer and end of life care: information for people in the last months, weeks and days of life.
You can also order a physical copy.

Published April 2021
Review date April 2024