Find out more about NHS England’s guidance on implementing a 21 day diagnostic pathway for pancreatic cancer:
"We need things to change if patients are going to stand a chance of living longer"
Pancreatic cancer is tough to detect. And even once it’s spotted, people can go on to face potentially huge obstacles: from getting diagnosed quickly, accessing treatment and having the support they need to manage symptoms.
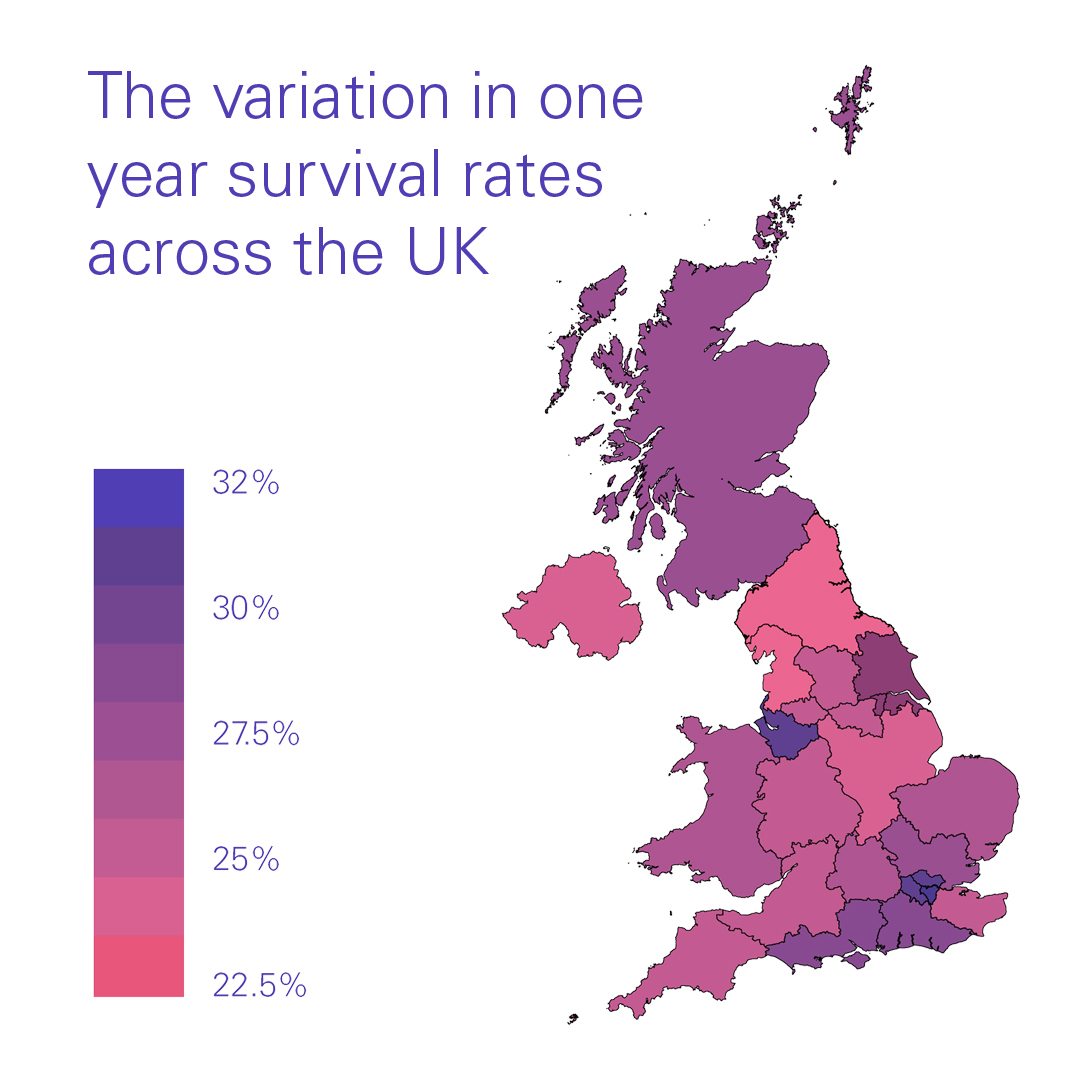
People face a postcode lottery of care depending on where they live in the UK and all these factors impact people with pancreatic cancer’s quality of life and chance of survival.
That’s why, in 2021 Pancreatic Cancer UK embarked on the Optimal Care Pathway initiative. We have brought together a community of health professionals and people with lived experience across the UK to understand the obstacles people face, and agree what needs to happen to improve diagnosis, treatment and care. You can find out more about our community here.
As one unified voice we have worked together to develop what an Optimal Care Pathway for pancreatic cancer should look like. Together, we have agreed three crucial areas in which we need to see improvements for people with pancreatic cancer:
- Fairer Care: Everyone should get advice, care and support from dedicated expert professionals from diagnosis
- Faster Diagnosis: Everyone should have their diagnosis confirmed or ruled out within 21 days of being sent for tests
- Faster Treatment: Everyone should start treatment within 21 days of diagnosis
Read more about our recommendations in our report
The Optimal Care Pathway report
We have developed a detailed report which outlines:
- What high-quality diagnosis, treatment and care looks like for people with pancreatic cancer and healthcare systems
- The impact better and fairer standards of care would have for people with pancreatic cancer and their loved ones
- What NHS systems and healthcare professionals across the UK can do to implement better and fairer standards of care
- Any gaps in evidence and research that still exist in some areas
Recommendations for NHS systems
As a community, we have agreed that NHS systems together with healthcare professionals across the UK can drive implementation of the Optimal Care Pathway by committing to delivering on 6 key recommendations, as laid out below, and expanded on throughout this report:
Our recommendations for better care
Recommendation 1
NHS systems should ensure that from the point of diagnosis and throughout a patient’s care, everyone with pancreatic cancer should be pro-actively offered support and care tailored to their needs. This includes ensuring:
- Access to prehabilitation and rehabilitation services
- Access to better nutritional management and specialist dietetic services
- Access to better psycho-social support services
- Access to better post-resection follow up care for people living beyond pancreatic cancer
Recommendation 2
NHS systems should ensure that everyone with pancreatic cancer has access to a 24/7 rapid access enhanced care service to get support with the symptoms and side effects of their cancer. This model should be a service delivery and rapid referral hub with close links to other specialist, secondary and local healthcare teams.
Recommendation 3
NHS systems should ensure that everyone with pancreatic cancer, regardless of where they are treated or cared for, has a hepato-pancreato-biliary or upper gastrointestinal clinical nurse specialist (HPB/UGI CNS) as their lead point of contact to oversee their care.
Our recommendation for faster diagnosis
Recommendation 4
NHS systems should ensure that everyone with pancreatic cancer is diagnosed within 21 days of referral for suspected cancer.
Our recommendations for faster, fairer treatment
Recommendation 5
NHS systems should ensure that treatment pathways are standardised depending on tumour classification and staging, so that everyone with pancreatic cancer has a fair chance of accessing life extending, or life-saving treatment.
Recommendation 6
NHS systems should ensure that treatment should be initiated within 21 days from confirmed diagnosis (and 42 days from referral) where appropriate, for people with pancreatic cancer.
How local health systems and healthcare professionals can drive implementation
Pancreatic Cancer UK and the Optimal Care Pathway expert community would like to work with local systems (e.g. Cancer Alliances, integrated care boards, cancer networks and health boards) and health professionals to embed our 6 recommendations for improvement.
Local health systems and health professionals should work together to:
- Develop business cases for local commissioners and national decision-makers to receive funding to implement improvements in pancreatic cancer care. Funding may include to increase workforce, dedicated expertise and resource for people with pancreatic cancer.
- Increase awareness and educate healthcare teams to implement better and fairer standards of care for people with pancreatic cancer as laid out in this report.
- Engage with existing and future national health improvement programmes in pancreatic cancer, such as the Getting It Right First Time for pancreatic cancer, the National Pancreatic Cancer Audit, the NIPANC/Queen’s University Belfast pancreatic cancer audit and future pancreatic cancer audits and health improvement programmes such as Prehabilitation for Scotland in Scotland.
Read our full recommendation in the report
Join our new Cancer Alliance Bulletin
Keep up to date with how you can drive improvements in pancreatic cancer pathways and care in your area.
Find out more about our guidance on optimal psychosocial support for people with pancreatic cancer:
We're calling on governments to make this pathway a reality
We recognise that for the Optimal Care Pathway to be fully implemented across the country, NHS systems will require sustained, additional funding from governments and national NHS organisations.
That’s why we’re calling on governments and national NHS organisations to make this happen.

