

Audit reveals people with pancreatic cancer are waiting too long for treatment costing thousands their chance of survival
New data published in the second annual National Pancreatic Cancer Audit (NPaCA) has revealed that people with pancreatic cancer in England and Wales are waiting too long for treatment to start, contributing to shockingly low treatment rates.
We are concerned about the continuing lack of progress in improving outcomes which is costing thousands their chance of surviving a diagnosis.
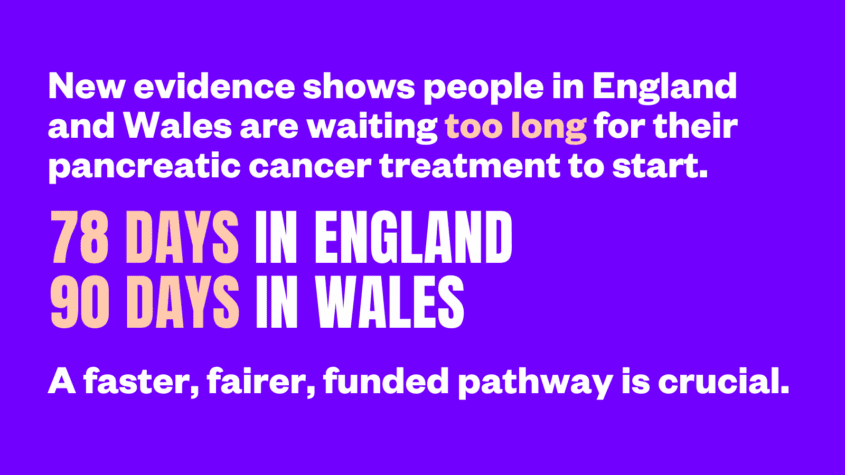
The 2025 NPaCA found that people with pancreatic cancer in England are waiting 78 days and in Wales, 90 days, for treatment to start following a GP referral. The NHS target is 62 days.
Waiting times for pancreatic cancer treatment have got even longer compared to last year’s audit which included people diagnosed in 2020 and 2021: patients in England are waiting an additional 3.5 days and 8 days in Wales for treatment to start.
Treatment rates for the disease also remain unacceptably low – particularly among people diagnosed early when the disease is most treatable. Of those diagnosed at stages 1-3, just 57% received any sort of treatment in England and 51% in Wales.
This figure drops considerably for people diagnosed with incurable pancreatic cancer (stage 4), with only 27% receiving any treatment in England and 24% in Wales. The disease has the lowest treatment rate (34%) of any common cancer- comparing poorly with treatment rates for breast (86%), bowel (74%) and lung (56%).
In England and Wales, around 10,000 people are diagnosed with pancreatic cancer each year. Over half will die within three months of diagnosis. Devastatingly, a person diagnosed today has a similar chance of survival as someone in the 1970s. The disease can progress rapidly and, tragically, 80% of people are diagnosed too late for lifesaving surgery to remove the cancer.
To give people with a terminal diagnosis more invaluable time with their loved ones, we believe it is imperative they are given access to life-extending treatment faster than the current NHS target of 62 days, before their health deteriorates too much to tolerate it.
"The NHS desperately needs the staff, resources and investment to ensure it is prepared to implement the improvements needed to change survival."
Our charity contributed and helped launch the NPaCA last year, which aims to better understand the state of pancreatic cancer care. The audit helps to shape guidelines and pathways like the Optimal Care Pathway which our charity designed with input from healthcare professionals and people impacted by the disease.
If the Optimal Care Pathway was fully implemented, it would reduce variation and improve the diagnosis, treatment and care for people with pancreatic cancer.
We hope the findings from the 2025 NPaCA will prompt the UK Government to make desperately needed improvements through the National Cancer Plan, and support healthcare professionals to implement them.
Following the audit, we are calling for:
- The development and implementation of national, timed, optimal pathway for pancreatic cancer. The pathways would supersede outmoded guidance and provide a strategic, central vision for optimal treatment and care for local healthcare systems to deliver
- Appointing a national role to support the implementation of urgently needed local pathway improvements throughout the journey of someone with pancreatic cancer.
- Sustained funding for the specialist roles involved in caring for people with pancreatic cancer – including a commitment to increase the number of Clinical Nurse Specialists and cancer navigators, who provide crucial personalised support for people impacted by the disease
The 2025 NPaCA also found that more people with pancreatic cancer were waiting longer than 21-day timeframe from urgent GP referral to receive their diagnosis recommended by NHS guidance, with 54% of those in England and 51% in Wales diagnosed within 21 days.
The NPaCA has now been running for two years, and we want to see it funded until survival rates drastically improve, so that insight specific to people with pancreatic cancer isn’t lost.
The audit will be invaluable in gauging the impact the upcoming National Cancer Plan has on diagnosis, treatment and survival of the disease. Prior to 2021, data for pancreatic cancer was amalgamated with hepatobiliary or upper gastrointestinal cancers making it difficult to identify recommendations to combat the unique challenges it poses.
Nations across the UK have started to make progress in combating these challenges thanks to our influence and our work on the Optimal Care Pathway. The Northern Irish Government are working with us to implement the pathway in the nation, and the Scottish Government has committed to improving survival of pancreatic cancer in its cancer strategy.
The UK Government has recognised the need for an optimal care pathway for people with the disease in England, however we now want to see the same national commitment to improve survival of the disease in the upcoming National Cancer Plan for England.
We also want to see understaffing issues throughout NHS Wales resolved quickly, to enable the system to better implement improvements and handle the rise in suspected cancer referrals.
"People with this disease deserve more than this. This continuing lack of progress across both diagnostic and treatment pathways for pancreatic cancer cannot be allowed to continue."
Prior research we conducted implied that implementing an Optimal Care Pathway, where people receive their diagnosis within 21 days of being sent for tests, and treatment within 21 days of diagnosis, could mean that 5,000 people get a chance to live longer.
The modelling we did in 2023 also suggested implementing the pathway could double all treatment rates for the disease, from 3 in 10 receiving treatment, to 6 in 10.
Alfie Bailey-Bearfield, Head of Influencing and Health Improvement for Pancreatic Cancer UK, said:
“For people with pancreatic cancer to still be experiencing unacceptable waits and that so few are receiving treatment, is completely devastating. Tragically, while waiting many become too unwell for treatment, depriving them of invaluable time they had left with their loved ones. People with this disease deserve more than this.
“This continuing lack of progress across both diagnostic and treatment pathways for pancreatic cancer cannot be allowed to continue. The NHS desperately needs the staff, resources and investment to ensure it is prepared to implement the improvements needed to change survival. We need to see swift action from UK Governments in supporting our health systems so that we can finally give people with pancreatic cancer more than hope in the future.”
