Pancreatic neuroendocrine cancers
Pancreatic neuroendocrine cancers are also known as pancreatic neuroendocrine neoplasms (pNENs).
What's in the 'Types of pancreatic cancer' section?
What are pancreatic neuroendocrine cancers?
There are two types of pancreatic neuroendocrine neoplasms (pNENs). These are pancreatic neuroendocrine tumours (pNETs) and pancreatic neuroendocrine carcinoma (pNECs).
- Pancreatic neuroendocrine tumours (pNETs) can grow at different rates. Some may grow slowly, but others may be fast growing.
- Pancreatic neuroendocrine carcinomas (pNECs) are much less common. They grow quickly and cause symptoms similar to PDAC.
We use the term pancreatic neuroendocrine cancer for both. But they behave differently and are treated differently, so speak to your doctor about whether your cancer is a pNET or pNEC.
We don’t know why most neuroendocrine cancers happen. But a very small number of rare inherited genetic conditions are linked to pancreatic neuroendocrine cancer.
Neuroendocrine Cancer UK have more information about diagnosis, treatments, and living with neuroendocrine cancers, including pNETs and pNECS.
Where do neuroendocrine cancers develop?
Neuroendocrine cancers develop in neuroendocrine cells, which are found in different organs or parts of the body. Neuroendocrine cells make hormones that help to control how our bodies work.
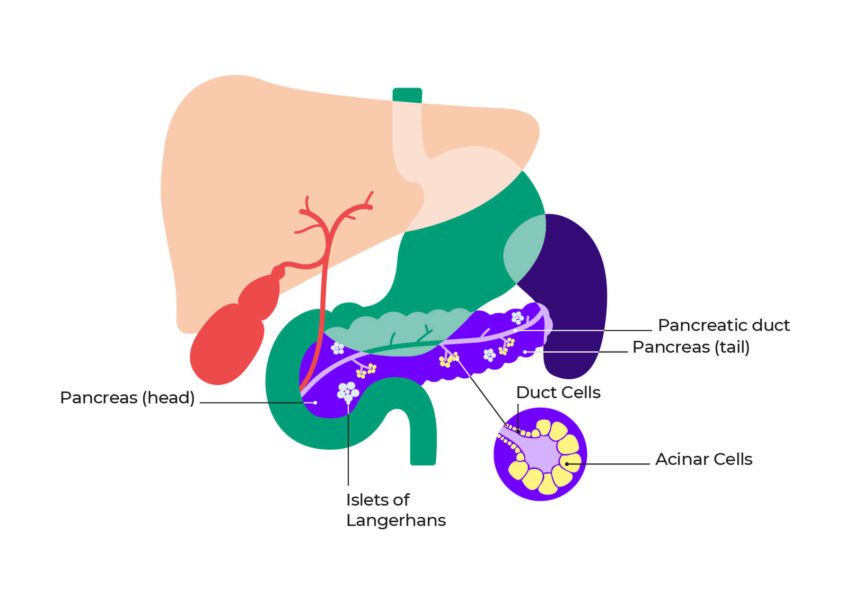
Pancreatic neuroendocrine cancers start in cells in the pancreas called Islets of Langerhans (see diagram below). These cells make hormones, including insulin and glucagon, which control the sugar levels in the blood.
Diagram showing the anatomy of the pancreas
Pancreatic neuroendocrine cancers may be called functioning or non-functioning. This depends on whether they produce higher levels of hormones, which cause symptoms. Most are non-functioning. This means that they don’t produce more hormones than normal.
Non-functioning pancreatic neuroendocrine cancers
Most pancreatic neuroendocrine cancers (60-90%) are called non-functioning neuroendocrine cancers. They don’t make higher than normal levels of hormones. This means they do not have symptoms related to hormones.
Non-functioning neuroendocrine cancers may be harder to detect and diagnose than functioning neuroendocrine cancers. This is because they may not cause symptoms. If they do cause symptoms, these may include symptoms similar to PDAC, like indigestion or weight loss. Non-functioning neuroendocrine cancers are often diagnosed during tests for another problem.
Functioning pancreatic neuroendocrine cancers
Some pancreatic neuroendocrine cancers produce higher levels of certain hormones, which can cause specific symptoms. These are called functioning neuroendocrine cancers. Up to 40 in 100 (40%) pancreatic neuroendocrine cancers are functioning.
Insulinomas
Insulinomas are pNETs that can occur anywhere in the pancreas. They make too much of the hormone insulin, causing low blood sugar levels. Low blood sugar levels can cause symptoms like dizziness, light headedness, sweating, hunger, confusion and irritability. People sometimes put on weight due to eating more because they feel hungry.
Up to 30 in 100 insulinomas (30%) are linked to an inherited genetic syndrome called multiple endocrine neoplasia type 1 (MEN1).
Gastrinomas
Gastrinomas are pNETS that are found in the pancreas and the duodenum (the first part of the small intestine). They produce too much of a gut hormone called gastrin. High levels of gastrin means that too much stomach acid is made.
Symptoms may include chest and/or tummy pain, acid reflux, heartburn, diarrhoea and tiredness. These combined symptoms are called Zollinger-Ellison syndrome. Too much gastrin may also cause irritation of the stomach or duodenum, leading to ulcers and bleeding.
Up to 30 in 100 gastrinomas (30%) are linked to an inherited genetic syndrome called multiple endocrine neoplasia type 1 (MEN1).
Glucagonomas
Glucagonomas are pNETs that are mostly found in the body and tail of the pancreas. They make too much of the gut hormone glucagon, which helps to control blood sugar levels.
Symptoms include a distinct type of skin rash (redness and blisters), particularly on the face, tummy, bottom and feet. Other symptoms of glucagonomas include:
- diabetes (high blood sugar levels)
- diarrhoea (runny poo)
- weight loss
- changes in mood
- anaemia (low levels of red blood cells)
- blood clots
- a sore mouth and tongue.
Less than 10 in 100 glucagonomas (10%) are linked to the rare inherited genetic syndrome called multiple endocrine neoplasia type 1 (MEN1).
VIPomas
VIPomas are pNETs that are more commonly found in the tail of the pancreas. They make too much of a hormone called vasoactive intestinal peptide (VIP). VIP normally helps to neutralise stomach acid and control how quickly food passes through the bowel.
Symptoms include lots of watery diarrhoea, dehydration, low levels of potassium in the blood (hypokalaemia), tummy pain, bloating, and a flushed face.
Other functioning pancreatic neuroendocrine cancers include:
- Somatostatinomas which produce too much somatostatin. This can lead to symptoms including gallstones, steatorrhoea (pale, oily poo), anaemia, tummy pain, high blood sugar levels and jaundice.
- ACTHomas which produce too much ACTH (adrenocorticotropic hormone). This can cause symptoms of Cushing’s disease, including weight gain, easy bruising, anaemia, depression, increased risk of infection and darkened skin.
- PTHrPomas which produce too much PTHrP (parathyroid hormone-related protein). This can cause symptoms including high calcium levels, tummy pain, feeling and being sick, constipation, bone pain, osteoporosis, fatigue, and confusion.
- Ppomas which produce too much pancreatic polypeptide. This can cause symptoms including diarrhoea, abdominal pain and weight loss.
Finding out more
Speak to your medical team with any questions about pancreatic neuroendocrine cancers and how they are treated.
Neuroendocrine Cancer UK have more detailed information and lots of support around diagnosing, treating and living with pancreatic neuroendocrine cancer. This includes a helpline with specialist nurses, peer support and a dedicated neuroendocrine cancer counselling team.
Questions to ask your doctor or nurse
- What type of pancreatic neuroendocrine cancer do I have?
- Is it a neuroendocrine tumour or a neuroendocrine carcinoma?
- Is it functioning or non-functioning?
- How is this type of neuroendocrine cancer treated?

References
We have listed some of the references to the sources used to write this information. If you would like the full list of references, email us at publications@pancreaticcancer.org.uk
- Albers MB et al. Characteristics, therapy, and outcome of rare functioning pancreatic neuroendocrine neoplasms. Sci Rep 14, 18507, 2024. https://doi.org/10.1038/s41598-024-68290-1 [Accessed June 2025]
- Clancy T. Surgical Management of Pancreatic Neuroendocrine Tumors. Hematol Oncol Clin N Am. 30:103-118, 2016. doi: 10.1016/j.hoc.2015.09.004 [Accessed June 2025]
- Kelgiorgi D and Dervenis C. Pancreatic neuroendocrine tumors: the basics, the gray zone, and the target. F1000Research. 6(F1000 Faculty Rev):663, 2017. doi: 10.12688/f1000research.10188.1 [Accessed June 2025]
- Nagtegaal ID et al. for the WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology, 76(2):182-188, 2019. doi: 10.1111/his.13975 [Accessed June 2025]
- Pavel M et al. Gastroenteropancreatic Neuroendocrine Neoplasms: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-up. Ann Oncol 31(7):844-60, 2020. doi: 10.1016/j.annonc.2020.03.304 [Accessed June 2025]
Published August 2025
To be reviewed August 2028
