What's in the 'Surgery for pancreatic cancer' section?
There are different operations for pancreatic cancer. They involve removing part or all of the pancreas. The type of surgery you have will depend on where the cancer is in the pancreas and how much of the pancreas is affected. The surgeon may also need to remove other organs and tissues around the pancreas.
The types of surgery are called:
- Whipple’s procedure
- Pylorus-preserving pancreaticoduodenectomy (PPPD)
- Distal pancreatectomy
- Total pancreatectomy
- Removing part of a vein (vein resection)
Your surgeon will explain which operation is suitable and what will happen. Ask them if you have any questions.
Whipple’s operation (pancreatoduodenectomy or PD)
The Whipple’s procedure is the most common type of surgery for pancreatic cancer. It is used for cancers in the head or neck of the pancreas.
During a Whipple’s operation, the surgeon will remove:
- the head of the pancreas
- the lower end of the stomach
- the duodenum (first part of the small intestine)
- the gallbladder (which stores a fluid called bile, which helps digestion)
- part of the bile duct (which carries bile from the liver to the duodenum)
- some of the nearby lymph nodes (part of the immune system).
The surgeon will then join the remaining part of the stomach and bile duct to the small intestine. The pancreas is joined to the small intestine or to the stomach.
You may have an operation that’s like a Whipple’s, but none of the stomach is removed. This is called a pylorus-preserving pancreatoduodenectomy (PPPD).
Diagram showing the parts of the body removed by a Whipple’s operation:
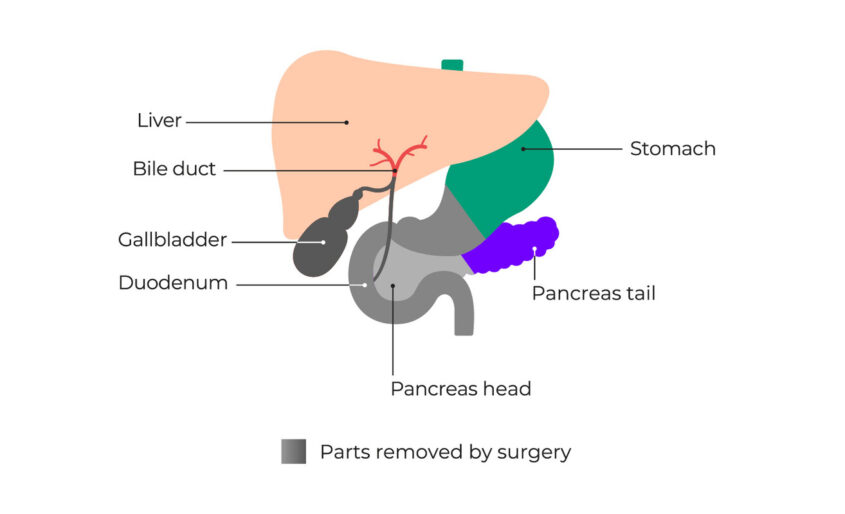
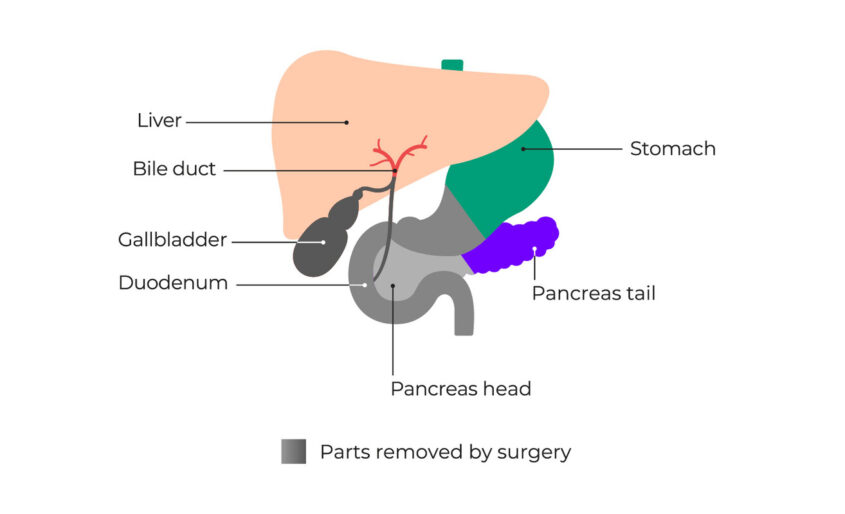
Diagram showing the pancreas and nearby organs after a Whipple’s operation:
As part of your pancreas is removed during the Whipple’s operation, this may affect your digestion. You may need to take capsules when you eat that contain enzymes that help you digest your food. This is called pancreatic enzyme replacement therapy (PERT). You might also get diabetes after a Whipple’s procedure – this can happen at any time after your operation. Read more about side effects of a Whipple’s operation.
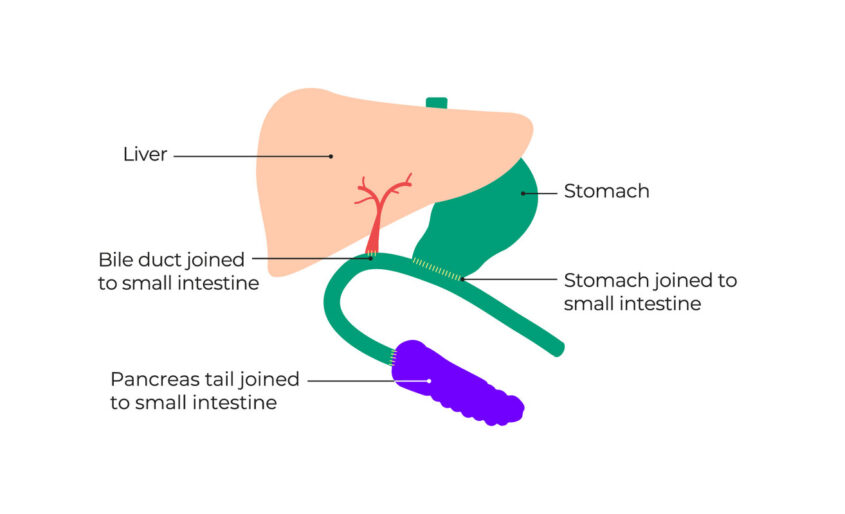
Distal pancreatectomy
A distal pancreatectomy removes the body (middle) and tail of the pancreas. The surgeon removes the spleen as well. This part of the operation is called a splenectomy.
Diagram showing the parts removed by a distal pancreatectomy:
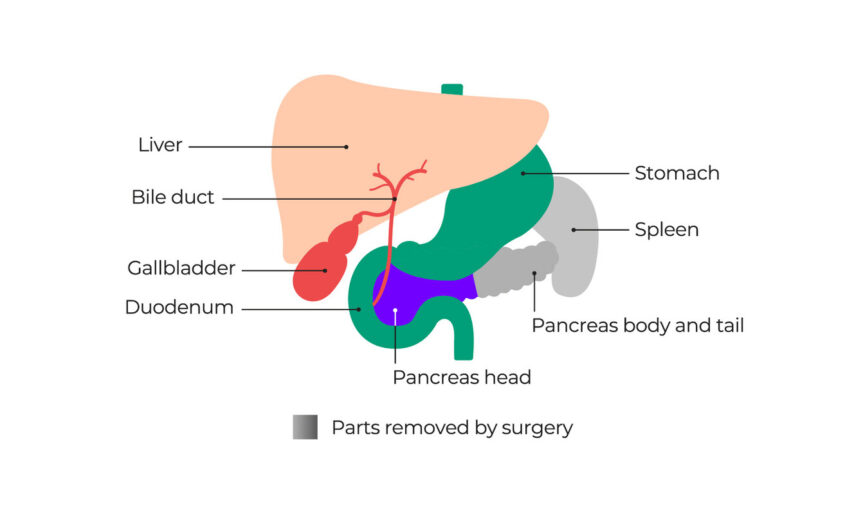
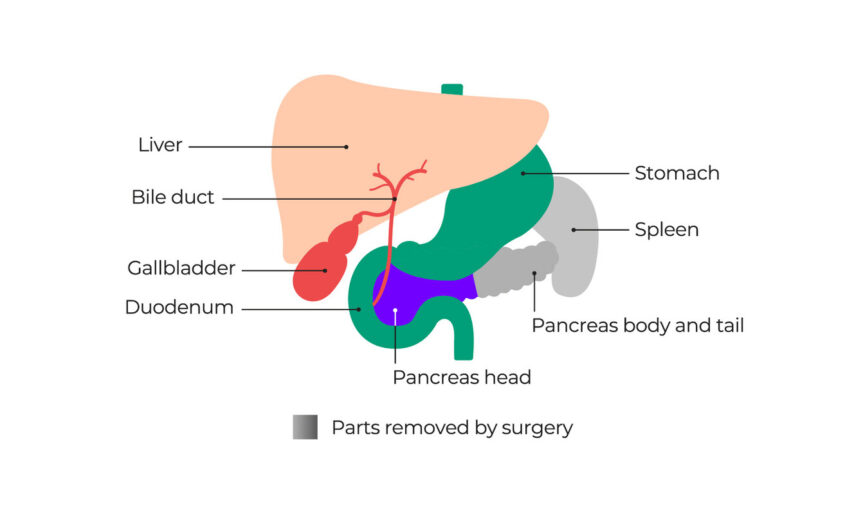
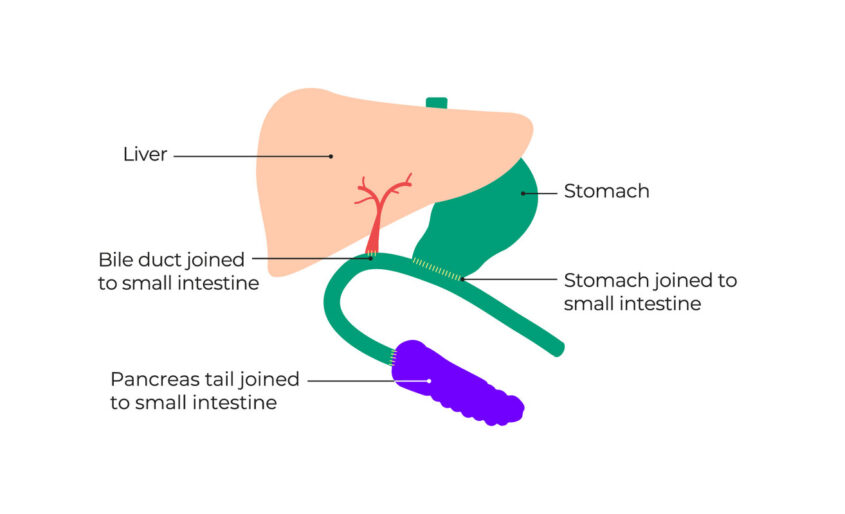
Diagram showing the pancreas and nearby organs after a distal pancreatectomy:


You are more likely to get diabetes after a distal pancreatectomy. You may need medicine to manage this. Your digestion may also be affected after a distal pancreatectomy, but this is less likely than after a Whipple’s operation. If your digestion is affected, you may need to take pancreatic enzyme capsules.
The spleen helps your body fight infections, so you are more likely to get infections if it is removed. You will need vaccinations to help protect against these. You may also need to take antibiotics for the rest of your life. Ask your doctor or nurse about vaccinations and antibiotics. You can carry a card saying you have no spleen, in case you become ill. Go to GOV.UK to get one.
Read more about possible side effects of a distal pancreatectomy.
Total pancreatectomy
You may have a total pancreatectomy if the cancer is large, or you have more than one tumour in your pancreas. The surgeon will remove:
- the whole pancreas
- the duodenum
- the gallbladder
- part of the bile duct
- the spleen (see above).
The surgeon may also remove part of your stomach. This will depend on where the cancer is. They will then join the stomach and bile duct to the small intestine.
Diagram showing the parts removed by a total pancreatectomy:
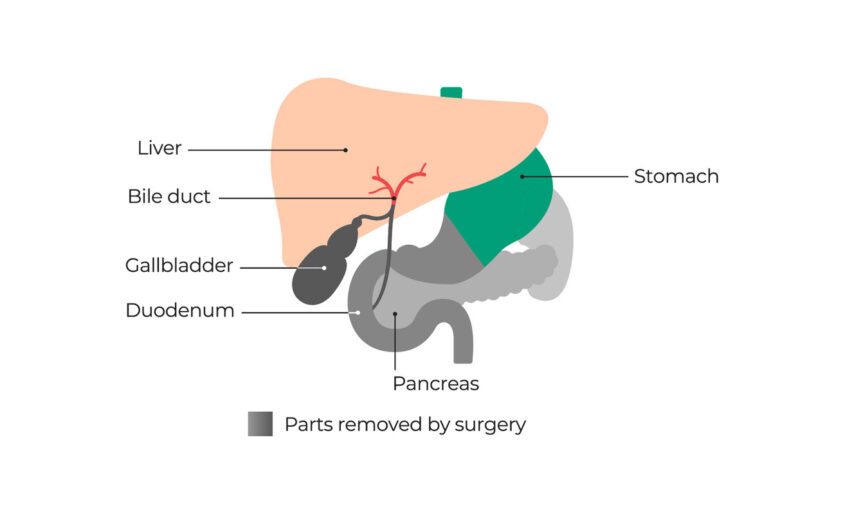
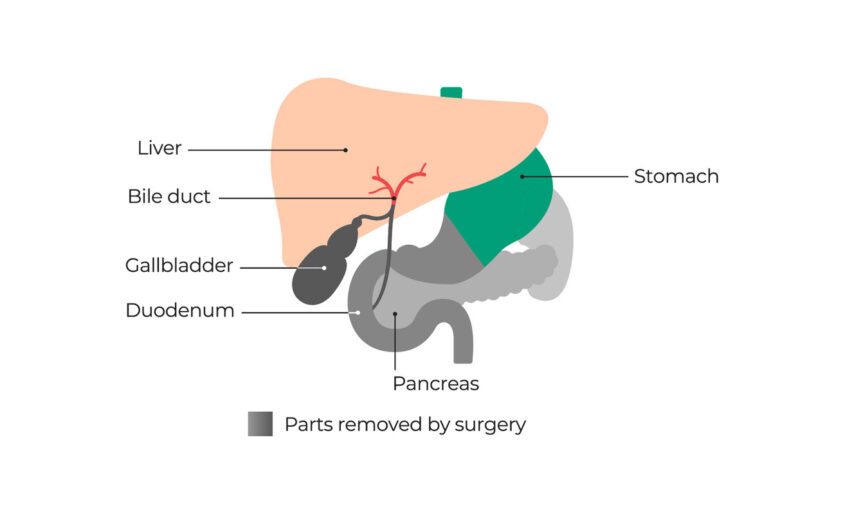
Diagram showing the organs after a total pancreatectomy:


As the whole pancreas is removed in a total pancreatectomy, you will need to take pancreatic enzyme capsules to help you digest food. You will also get diabetes and will need a medicine called insulin to manage this.
Read more about possible side effects of a total pancreatectomy.
Removing part of a vein
If the cancer has grown into or around major blood vessels near the pancreas, the surgeon may need to remove part of the vein. The vein is then joined back together. This is called vein resection and reconstruction. The surgeon may put in a piece of vein from somewhere else in the body or use an artificial material – this is called a graft.
Vein resection makes the surgery more complicated. You need to be very fit and well to have this type of surgery. If your surgeon is not sure if vein resection is possible, you could ask for a second opinion from another surgeon who is experienced in these.
The operation might not be available at your nearest specialist centre. You may be referred to another specialist centre to have the surgery.
Questions to ask your doctor or nurse
Which type of operation do I need?
What organs will be removed?
Will I need to take PERT or other medicines afterwards?
Updated January 2024
Review date January 2026

