Improving Outcomes Now: A look at our Virtual Annual Summit Sessions 2020
A summary of the highlights from this year's sessions exploring chemotherapy, nutritional care and the pathway from diagnosis to treatment.
2020 has been a particularly challenging year and back in March we had to postpone our Annual Summit. Determined not to lose the amazing momentum the pancreatic cancer community has gathered to find innovative solutions to maintain and improve treatment and care, we brought the Summit back in September covering the same vital topics through virtual sessions.
If you were unable to join the online sessions, read on for an overview of what took place.
Welcoming the pancreatic cancer community
We welcomed 527 attendees across the three virtual events, reaching more people than would ever have been possible at the physical event. The whole community came together, with health professionals, researchers, influencers, supporters and people affected by pancreatic cancer, joining from all over the UK and beyond, to play a role in improving outcomes for pancreatic cancer now.
Improving outcomes now
We explored three areas where we know variation in treatment and care currently exists and where tackling this variation could improve outcomes for patients. With this variation in mind, the core purpose of each session was to identify barriers to optimal care that exist within each area and to share tangible solutions to break these down.
1. Improving access to chemotherapy
Variation – what do we know?
Only 28% of people with pancreatic cancer have any form of chemotherapy. Only 50% of operable patients undergo chemotherapy after surgery, and only 25% of people with metastatic cancer receive chemotherapy, despite the evidence it can improve survival.
Breaking down the barriers
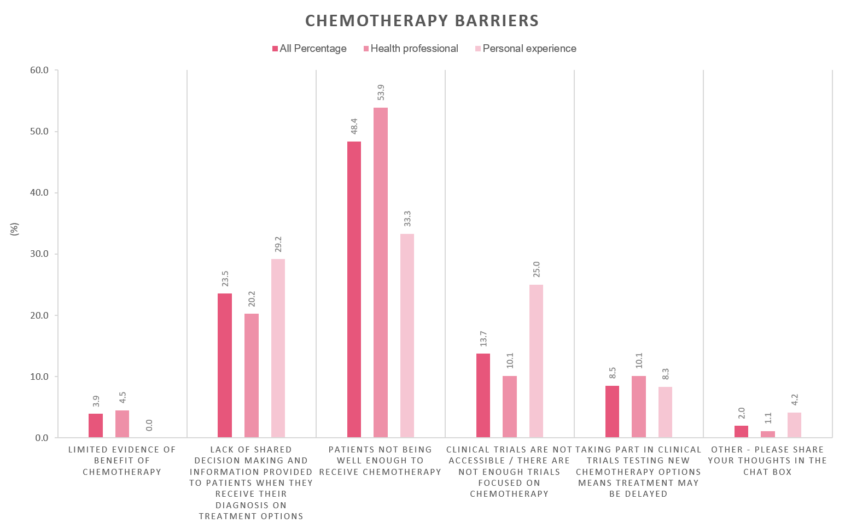
We asked attendees what they think is the biggest barrier to patients accessing chemotherapy. Nearly half of attendees, in particular health professionals, said patients not being well enough to receive chemotherapy is the main issue. A lack of shared decision making and patients not having enough information on treatment options to make decisions were also highlighted as key barriers.
Solutions for improvement
As solutions to improve the use of chemotherapy, we explored three areas: access to pancreatic cancer trials; the Bridging Clinic model in which patients receive information and symptom management early within their care; and a model of centralised specialised chemotherapy. You can find out more by watching the recording, viewing the slides or reading the key notes here.
We asked delegates which solutions (not limited to those presented) they think would have the biggest impact. Opinions were varied with health professionals saying greater focus should be put on prehabilitation to ensure patients are well enough for chemotherapy and people with a personal experience of pancreatic cancer saying that more and better access to clinical trials and more support for patients to participate in shared treatment decision making would make a big impact.
2. Improving access to optimal nutritional care
Variation – what do we know?
Pancreatic Enzyme Replacement Therapy (PERT) not only increases quality of life through managing digestive symptoms but it can also increase tolerance to treatment and significantly extend the life of pancreatic cancer patients by 3.8months. However, only 54% of people with pancreatic cancer are prescribed PERT and inoperable patients are less likely to receive PERT than those who undergo surgery (45% vs 78%) [RICOCHET, Unpublished Manuscript].
Personal experience
Macca joined us to share the challenges he faced in getting a PERT prescription. He lost over three stone within the space of four months and it took speaking to one of our Support Line nurses for him to find out about PERT and how it might help. When asked about the difference it made to him, he said quite simply that it meant he was able to eat, and as a result was able to put on weight to fight the cancer.
Breaking down the barriers
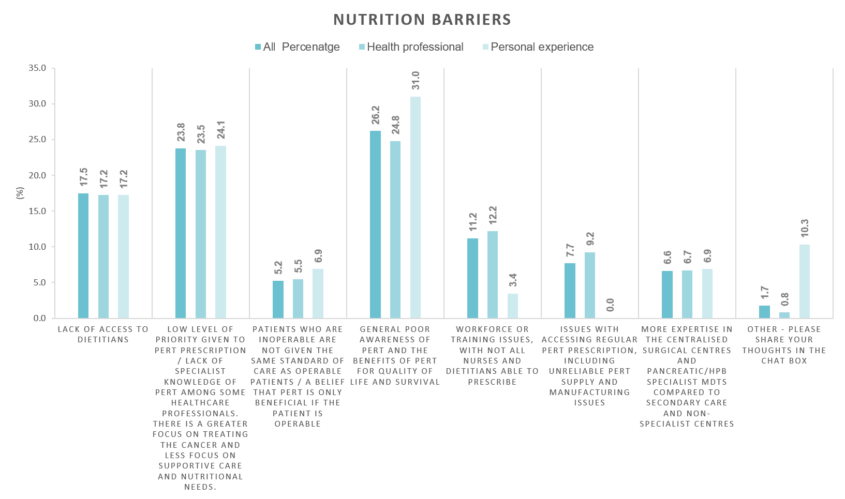
We asked attendees what the biggest barrier to patients accessing PERT is. Attendees were split but the main themes highlighted were poor awareness of PERT and the benefits, and a lack of specialist knowledge among some health professionals and more focus given to treatment than supportive care.
Solutions for improvement
As potential solutions to improve access to PERT and nutritional care we looked at how specialist dietitians can support local dietetic teams within secondary care, training dietitians as supplementary prescribers and a mobile health app to empower patients to ensure their nutritional symptom needs are met. Watch the recording, view the slides or read the key notes here.
Delegates voted on the solution they think would make the most significant impact. The majority said it would be for every patient to have access to a dietitian. Among people with a personal experience, nearly ¼ said that better general awareness and information about PERT and the benefits would have a big impact too.
3. Improving the pathway from diagnosis to treatment
Variation – what do we know?
We often hear through our Support Line and discussions with pancreatic cancer specialists that there is inconsistency in how care is delivered across the UK with delays occurring between diagnosis and treatment due to coordination problems between clinical specialists and different hospitals as well as a lack of standardised clinical pathways. The median pathway length between diagnosis and treatment is 24 days but this varies considerably depending on where in the UK you live, your age and the route to your diagnosis (e.g. A&E, GP referral etc). View the data here. This is a critical issue because longer waiting times to treatment have been shown to reduce the numbers having treatment and lead to worse survival outcomes.
Personal experience
In the pathway session, Claire shared her mum’s experience. After nine months of trips to the GP and multiple delayed and unsuccessful stents, when she was finally diagnosed with pancreatic cancer, it took a further three months for her treatment to begin. Claire said if she could make one change it would be for health professionals to communicate better between departments and look at the patients as a whole as her mum’s care was very segmented.
Breaking down the barriers
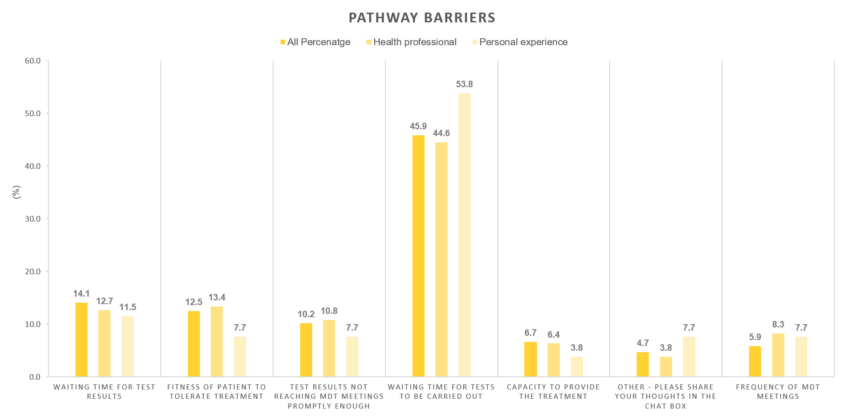
When we asked attendees what they think is the biggest barrier in a patient’s pathway to starting treatment, the majority said it is the waiting time for tests to be carried out.
Solutions for improvement
Solutions proposed to improve the diagnosis to treatment pathway were: improvements to how Multidisciplinary Teams operate and meeting frequency; a 14-day referral to treatment pathway; and early engagement of clinical nurse specialists to support pathway navigation. Find out more by watching the recording, viewing the slides or reading the key notes here.
Attendees said that introducing one stop clinics for all tests and investigations would make the most significant improvement.
Commitment to change
Our ambition was to inspire the community to unite and take action. We were delighted to see all the changes attendees committed to in the feedback. Here are a few of them:
“We will be looking into the great concept of the bridging clinic Mr Kumar discussed. This is an excellent idea and we will try to tailor this to each individual patient’s needs for information and support”
Attendee at Improving Access to Chemotherapy
“… The webinar has really impacted positively on my practice and therefore patient care. [I] Spent yesterday ensuring dietetic referrals were all actioned.”
Attendee at Improving Access to Optimal Nutritional Care
“My role includes working to improve cancer care across all the sites. This includes a newsletter to primary care, which includes some learning points – I will include a section on pancreatic cancer with some key points from these presentations.”
Attendee at Improving the Pathway from Diagnosis to Treatment
Great work in the community
Attendees also told us about some of the great work they’re already doing. Here are just some of their activities:
“Scotland has quality performance indicators for pancreatic cancer, including access to and uptake of chemotherapy.”
Attendee at Improving Access to Chemotherapy
“[I] Work in a secondary care centre… Our trust has 2 hospitals since it merged. One has dedicated oncology which includes pancreatic patients and the other has no dedicated oncology funding. We are putting forward a business case for dedicated oncology funding for the hospital without any and sessions like this help provide evidence for the business case.”
Attendee at Improving Access to Optimal Nutritional Care
“WY&H Cancer Alliance recently held a virtual meeting to discuss optimal pathway for HPB patients and the difficulties we encountered due to COVID. A number of workstreams will be developed from this – RDC`s, Personalised care agenda / interventions, standardizing communication.”
Attendee at Improving the Pathway from Diagnosis to Treatment
Improving outcomes now and in the future
At Pancreatic Cancer UK we are determined to work with the pancreatic cancer community to improve outcomes for everyone affected by pancreatic cancer in the UK. We have already begun building evidence of what optimal care looks like and over the next year will be working with health professionals and those affected by pancreatic cancer to define an optimal pathway. We are also seeking support from Governments across the UK for work to improve care for pancreatic cancer, and pushing for national cancer plans to prioritise this work.
If you have examples of best practice to share or would like to register your interest in helping us develop an optimal care pathway please get in touch.