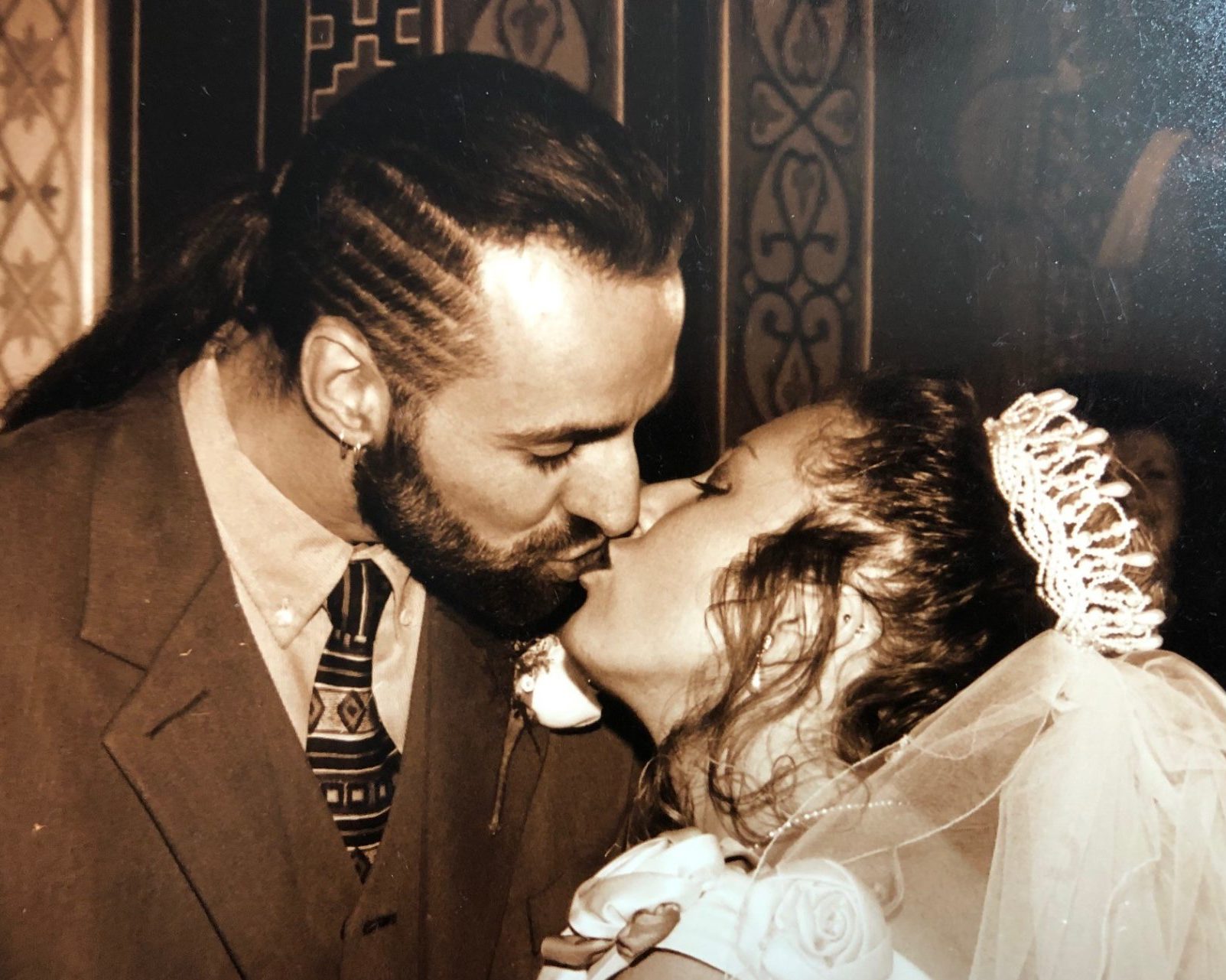
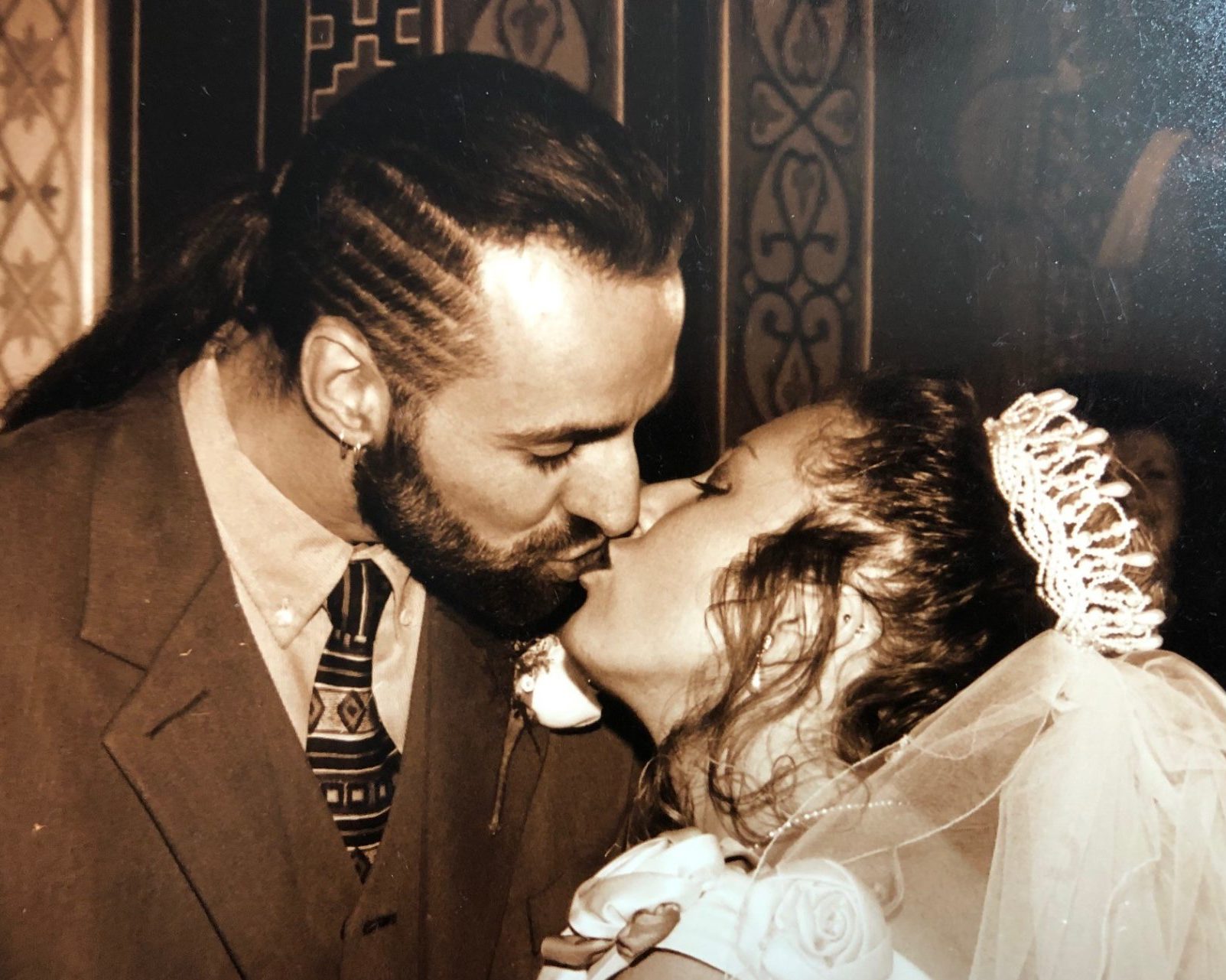


Sharon & Paul
Sharon shares the story of her husband Paul, who passed away at home with his family aged 51, just weeks after being diagnosed.
My beautiful husband, the person I shared the last 29 years (well over half of my life) with, Paul, was a 6 foot 4 giant of a man with a heart equally as big. He was extremely fit and healthy and working 6, often 7, days a week just 6 weeks before he died. He still played competitive football twice a week, went to his gym daily and regularly went out for a sprint on his bike. He was just 51 when he passed away.
We didn’t realise there was something wrong – but early signs were there
Having 3 kids and with both of us working full time, life was hectic. For several months prior to any other symptoms being apparent and months before his diagnosis, Paul was saying how tired he was. He used to come home from work in an afternoon and have 20 minutes sleep every day before heading off to collect the kids from school. We attributed his fatigue to our busy lifestyles, either always at work or being a taxi service for the kids, and thought nothing more about it. I actually used to laugh at him and tell him that he got lots more sleep than me with his daily afternoon nap so he shouldn’t feel tired!
Paul often used to deliver some amazing belches (which he and the kids found hilarious!), so we never really noticed as these became more frequent, louder, and longer than usual. He’d also started to feel bloated when eating and often said he couldn’t eat big meals like he used to. We just accepted this, thinking it was just ‘an age’ thing and perhaps a sign of his metabolism slowing down.
Seeking a diagnosis
It was in February 2021 that he started to complain of a toothache like pain in his stomach and he contacted the GP thinking he may have a stomach ulcer. It was mid-COVID pandemic, and we were in lockdown, but the GP arranged to see him and consequently referred him for blood tests.
Trying to get an appointment for a blood test took several weeks due to COVID, as did the results. The first results indicated a problem with his liver, prompting lots of questions about his alcohol intake. Like many people, Paul did enjoy a beer or two, but we knew that his symptoms were not caused by excessive drinking or addiction to alcohol, or to any other addiction. Paul was always considerate of his health, looked after himself and had never even tried a cigarette in his life! He chose what he ate carefully, and was not someone to put off going to the Doctor’s if he thought there was a problem. He wasn’t a ‘bury your head in the sand’ type. The results of a second set of blood tests, several weeks after the first, confirmed there was definitely something affecting his liver function. At this point the GP advised he would need a CT scan to get to the bottom of it.
More symptoms
Over the next few weeks, Paul deteriorated quickly. He was still pushing himself to go to work but the stomach pain had increased, and his fatigue meant he was sleeping more than before. He was already starting to eat less, was losing weight, and had now started to feel and be sick.
On the first day he felt too ill to go to work, I knew there was something seriously wrong. He never had time off, so I drove him to A&E myself but because of COVID I was unable to go in with him and explain how completely out of character this was. No appointment for a scan had arrived and I could see whatever was causing him to feel so ill needed addressing quickly. To most people, he would not have appeared seriously ill, a huge guy walking into A&E un-aided, but that was just because of how physically strong he was. It was not like him to complain when unwell or to stay in bed, but A&E sent him home and advised he needed to wait for the CT scan appointment to come through, advising there was nothing they could do until then.
Pushing to get help for Paul
Paul went back to work for a few more days, but in less than a week it was obvious his health was declining further. Whatever either of us were trying was not helping him get better. I called the GP and petitioned him to get Paul admitted to hospital. He asked many questions, including about his drinking habits, but he listened seriously to my concerns and accepted when I said this was not caused by alcohol abuse. The GP said he would speak to the hospital, but they were not taking in patients due to COVID so they may not admit him.
The GP saw Paul the same day and told him he could see signs of jaundice in his eyes and persuaded the hospital to admit him for further investigation. The GP came out to the car park with Paul where I waited for him, put his hand on my shoulder as he gave me the admittance letter, and said ‘You get him in.’
We both shared a few tears on that journey to the hospital as I told Paul it was the first step to getting him better and was what he needed. Neither of us wanted to be apart but we knew that our usual ‘home cures’ were not the answer this time. There was an unspoken concern that this might be more serious than we wanted to contemplate.
Tests in hospital during COVID
Paul spent 10 days on a liver ward, where the patients were mainly alcohol abuse patients. Paul had little rest as a consequence of the nightly noise and disturbances.
After a week in the hospital, he had a CT scan which revealed what they believed to be cancer in both his pancreas and liver, but he needed to stay a bit longer for a biopsy to confirm this.
Paul had walked into the hospital when he was admitted just 10 days earlier. But he was discharged in a wheelchair less than 2 weeks later, barely able to walk or talk and with the weight loss being visibly shocking, to await the conclusion of the results and the proposed treatment plan we were due to receive the following week.
Due to COVID, we had been unable to visit Paul during his stay in hospital, but I’d drive there daily and take the kids along whenever I could, so that we could meet him in the corridor or outside the building for just a few minutes whenever he felt up to it. He was never able to sit with us for long before needing to go back to the ward to lie down again. Seeing the change in him during this time was shocking and heart-breaking, we felt totally useless and so very far away.
Battling the pain
Paul was discharged to my care after this 10 day stay with no advice about what we needed to do, what to expect or who to call if there was a problem. There was no care plan and no pain management. They had given him oral morphine which was not manging his pain because he was being sick more frequently, so whatever medicines went in this way were not sticking around long enough to do the job they were intended to do.
That first night Paul was back at home was one of the worst days of my life, whatever medicines he was taking were doing little to help. Not knowing who to turn to, I called the paramedics. They arrived quickly and spent 4 hours with him, calling doctors to find better ways to control his pain. That week, whilst we waited for a confirmed diagnosis, was sickeningly difficult. I had promised Paul I wouldn’t let him be in pain, so our GP surgery were my new favourite hotline number and were having to come out to visit him on an almost daily basis.
Paul was re-admitted to hospital again only 5 days after coming home and still before we had received a confirmed diagnosis. This time they needed to drain fluid, which was building up in his stomach, giving him a very uncharacteristic pot belly as well as pain and discomfort.
His meeting with the consultant was booked for the following day, to discuss the conclusion of the multi-disciplinary team review of his biopsy results, and I was given permission to attend the meeting with him in the hospital.
Confirming the diagnosis of advanced pancreatic cancer
It was Friday 16th April 2021, only 3 weeks after our first trip to A&E, I’ll never forget that day. It was the same week our middle child, George, turned 16. The consultant came into the room to talk to us and, with Paul’s file in her hand, she gave us the news we’d both been dreading. It was pancreatic cancer which had spread to his liver. It was a small cell type cancer, ‘like lung cancer’, she said, and therefore it was very aggressive. The speed of advancement of the cancer meant he was deteriorating quickly.
The actual prognosis though, when it came, knocked everything out of the both of us, those words still haunt me: ‘Your kidneys have now started to fail so we can’t offer you any chemotherapy at this stage, you are very poorly, you don’t look well if you don’t mind me saying, I think you probably only have days to short weeks left, I’m sorry.’ Paul turned to me and said, very pragmatically, in his now whispered voice, ‘We don’t have long Duck, do we?’ There was no response I could give him.
Going home to our family
Paul was discharged later the same day as a fast-track patient, to be able to spend his remaining time at home with his precious family in the home he loved. That was the hardest thing we ever had to do together as parents, to go home and tell our 3 children who were just 11, 16 and 18 and had been waiting at home all day for news, that their Dad, the person who’d always been at the centre of their world, the rock for all of us, had only weeks (at best) left to live. Paul was adamant he wanted to support me by telling the kids together, despite it being almost midnight when we arrived home from the hospital and him being so very tired.
The discharge process this time was a whirlwind (unlike his discharge 6 days earlier). Paul was fitted with a syringe driver so that his medication could be intravenously administered, which the district nurses would come and replenish daily. And we were referred to numerous support services, so I had people to go to for help and support 24 hours a day if needed. Within 12 hours of being home, we had all sorts of equipment delivered to help me with his care, all of which he refused to use – with the exception of the adjustable bed we had installed downstairs, and he moved between our bed upstairs to the hospital bed in the living room, to help relieve his discomfort.
Making the most of our remaining time together
We all wanted to make the most of the time we had left, although Paul spent much of the time asleep, and his strength declined daily. The kids would come home from school and would lie with him on the bed, just holding his hand, wanting to be near him.
Paul remained mobile (with assistance) right to the end. His ‘last hurrah’ came in the week running up to his passing away, and it said so much about his character and what a mentally and physically strong person he was. He asked me one evening to get him downstairs. I was reluctant, believing he wasn’t strong enough. He didn’t have the strength or energy to argue and he knew he couldn’t make it without my help so, when he asked me again at 5.00 the next morning, I told him I’d find a way if that’s what he really wanted to do. With the help of our eldest Son, Jack, we got him downstairs to the kitchen where he sat watching the sunrise through the window as the fox ate her breakfast on our garden wall. I went back upstairs for just a few minutes and when I came back down, they were both enjoying a glass of lager and black together as if it was the norm at 5.15 every morning!
Paul passed away on Saturday 8th May 2021, just days after his last beer and only 3 weeks after his diagnosis. His appointment for the CT scan the GP had requested didn’t arrive until after he had passed away, the process and waiting time was just too long at every stage for this dreadful disease. The delays due to COVID and the length of time it took to complete 2 sets of blood tests just hadn’t helped us to get a diagnosis early enough to be able to start any treatment or to buy us any quality time together.
Consequently, our family are heartbroken and still learning to come to terms with life without him. My children are having to negotiate teenage life without their Dad and best friend and I’m without my rock, my anchor and soulmate. It’s just such a devastating, cruel and painful disease. I said to him many times I wished I could swap places with him and take it all away, he simply replied, ‘Don’t be daft Duck, I’m just pleased it’s me and not you.’ He was always selfless.
Remembering Paul
I’m so very proud of Paul, for the life he led, for the fantastic person he was, for the way he enriched our lives and for the way he faced pancreatic cancer, with courage and determination. Knowing it was far too late to be able to treat his cancer but resolutely determined to do things his way.
But no family should have to face this. I know we‘re not alone, it happens to thousands of others too (Paul said), but we must continue to raise awareness about the almost silent cancer killer that is pancreatic cancer. We were so in the dark about the symptoms but with hindsight, perhaps there were signs, we just didn’t know that at the time. The tiredness, the belching, the bloating, the loss of appetite and then the stomach pain, the weight loss and the vomiting. Had we acted sooner, things may have been different. Whilst we can’t turn back the clock, we can try and help others by telling our story and making sure that people are aware of the signs and encourage them to seek medical help immediately if they experience any of these symptoms.
We’re also lighting up purple this November, 2021, to help raise awareness of pancreatic cancer and we’re having a memories party and fundraiser on his birthday, 20th November. Many people walking past our house and seeing the banner and lights have asked me about it and I’ve been able to share and, hopefully, educate them just a little. Network Rail, based at Pride Park in Derby, where he worked for over 30 years, are also lighting up. Together, like thousands of others, we will help to spread the message about this most vicious disease and, with the help of fundraising, we will work tirelessly to combat this cancer and to help all those affected by it, but most of all to prevent anyone else having to experience the pain, loss, and heartbreak that we are suffering.
We will always love you Paul, today, tomorrow, and forever!
November 2021




