On this page you will find information about:
Each hospital may do things slightly differently, and treatment will vary depending on your cancer. Speak to your doctor or nurse about your treatment.
Gemcitabine is one of the main chemotherapy drugs used to treat pancreatic cancer. It can be given on its own, or with another chemotherapy drug called capecitabine (Xeloda®).
This is known as GemCap:
Each hospital may do things slightly differently, and treatment will vary depending on your cancer. Speak to your doctor or nurse about your treatment.
GemCap can be used in different ways.
If you are not well enough to cope with GemCap you may be offered gemcitabine alone, as it may have fewer side effects.
Gemcitabine can also be given with the chemotherapy drug nab-paclitaxel (Abraxane®) to treat advanced pancreatic cancer.
Talk to your doctor or nurse about which chemotherapy may be best for you.
You will have gemcitabine at the hospital as an outpatient. This means that you will go into hospital for treatment, but you will not need to stay overnight.
Gemcitabine is given in a four week cycle. This means you will have gemcitabine once a week for three weeks, and then have a break for a week. This break allows your body to recover. The number of cycles you have will depend on how the treatment is working, and how chemotherapy affects you. Your chemotherapy team can tell you more about this.
Gemcitabine is given as an infusion into a vein. You may hear an infusion called a ‘drip’. You will have an infusion of gemcitabine through a cannula. The infusion takes 30 minutes.
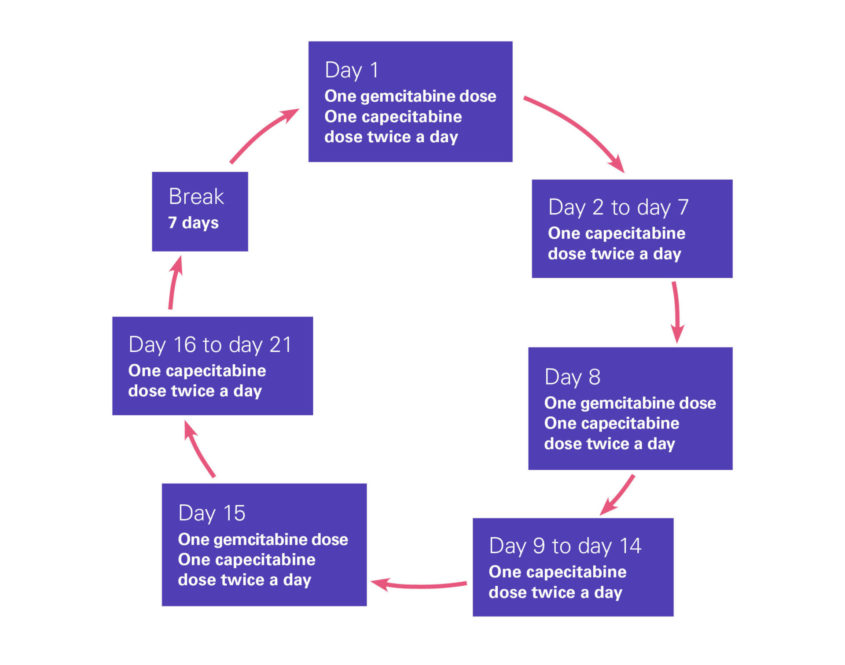
If you are having gemcitabine together with capecitabine (GemCap), this is given in a four week cycle. You will have an infusion of gemcitabine once a week for three weeks. Capecitabine is taken as tablets, which you will take twice a day for the three weeks. You will then have a one week break before starting the next cycle.
Diagram showing how GemCap is given
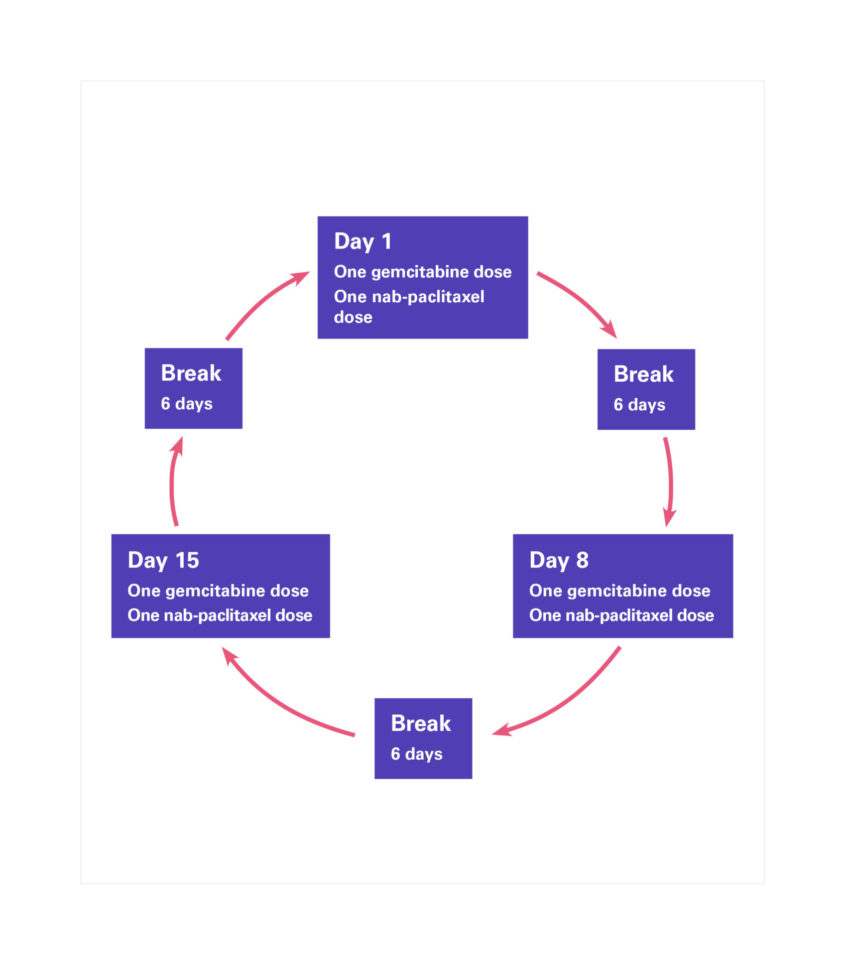
Gemcitabine with nab-paclitaxel (Abraxane®) is given in a four-week cycle. You will have an infusion of these drugs once a week for three weeks. You will then have a one week break.
Normally, both drugs are given on the same day. You will have an infusion of nab-paclitaxel for 30 minutes. After this, you will have a 30 minute infusion of gemcitabine.
Diagram showing how gemcitabine and nab-paclitaxel are given
Some people have a reaction while gemcitabine is being given. Signs of a reaction are:
If you have any of these or any other unusual symptoms, tell your chemotherapy team, as a reaction needs treating straight away.
Gemcitabine can cause side effects, but these can affect everyone differently, and you may not get all the side effects mentioned here.
Your chemotherapy team should tell you about any possible side effects and how they are managed. Ask them any questions you have. You can also speak to our specialist nurses on our free Support Line.
Most people cope well with gemcitabine but knowing what to expect can help you to deal with any side effects.
Your chemotherapy team should give you a 24 hour emergency number to call if you are unwell, have any signs of infection, or if you need information about any side effects. Your nurse will explain when to use this number. If you haven’t been given a number, ask your nurse about this.
Gemcitabine can increase your risk of getting an infection. An infection is an emergency if you are having chemotherapy, and needs treating straight away. Signs of an infection include:
Call the 24 hour emergency number your chemotherapy team will have given you if you have signs of an infection. You should phone if you have any of these symptoms or feel suddenly unwell, even if your temperature is normal or low.
Read more about infections and how they are treated.
While you are being given gemcitabine you may get some flu-like symptoms, such as feeling hot, cold or shivery, and having a headache. If these symptoms happen within 24 hours of having an infusion of gemcitabine, they may be a side effect of gemcitabine. You should still call the emergency number to check.
This is a common side effect of gemcitabine. You will normally be given anti-sickness medicines before your chemotherapy starts. If these medicines don’t help, speak to your chemotherapy team about changing to a different medicine. We have tips for coping with feeling and being sick.
Fatigue is a common side effect of gemcitabine. It is not the same as feeling tired. Fatigue can make you feel weak and have problems concentrating. Some people find that the fatigue starts a few hours to a few days after having chemotherapy and starts to get better after a few days. See how the chemotherapy affects you and work out how much activity you can manage. There are things that can help with fatigue. Read our tips on coping with fatigue.
If you have diarrhoea, try to drink as much water as you can. If you are finding it hard to drink enough fluids, contact your chemotherapy team. If you have diarrhoea more than four times a day, tell your chemotherapy team. They can give you medicines to control it. Read more about diarrhoea and how it is treated.
Constipation is when you find it harder to poo. Drink as much water as you can manage and try to eat foods that are high in fibre, such as fruit and vegetables. Gentle exercise such as walking can also help. Speak to your doctor about medicines that can help.
Gemcitabine can lower the number of red blood cells in your blood. This is called anaemia, and can make you feel tired, dizzy or short of breath. If any of these symptoms happen suddenly, call the emergency number.
Gemcitabine can lower the number of platelets in your blood. This is called thrombocytopenia. It can cause you to bruise more easily than normal, and you may be more likely to have nosebleeds or bleeding gums. If you have a nosebleed that does not stop after five minutes, call the emergency number.
Some people get swelling in their feet, ankles, legs, fingers or face. This is because of a build-up of fluid, which is called oedema. This normally gets better by itself. If you have swelling in your feet, it may help to have your legs up on a cushion when you are sitting down. Tell your doctor or nurse, as they may also give you medicines to help.
During your treatment you may not feel like eating, and you may start to lose weight. Try to eat small meals often. If your appetite doesn’t get better after a few days, tell your doctor or dietitian. We have tips on dealing with a poor appetite.
Gemcitabine can make your mouth sore, or cause mouth ulcers which can be painful. Tell your chemotherapy team about any problems with your mouth. They can make sure you don’t have a mouth infection, and give you a mouthwash which should help. You should also tell them if you have white spots in your mouth. This is a sign of oral thrush, which is normally easy to treat.
Gemcitabine may cause your hair to thin – but it should grow back once your treatment stops.
Gemcitabine can affect how your kidneys and liver work. You will have regular blood tests to check this. It usually goes back to normal after treatment ends.
Gemcitabine can cause an irregular heartbeat. It can also make you feel short of breath or dizzy. If you have any of these symptoms, call the emergency number. Or go to A&E and tell them that you are having chemotherapy.
Gemcitabine can cause an irregular heartbeat. It can also make you feel short of breath or dizzy. If you have any of these symptoms, call the emergency number. Or go to A&E and tell them that you are having chemotherapy.
Speak to your chemotherapy team if you feel anything unusual, or if you would like more information.
You can also speak to our specialist nurses on our free Support Line about gemcitabine and side effects.

You can download our fact sheet about Gemcitabine for pancreatic cancer.
Updated April 2022
Review date April 2024