On this page you will find information about:
Each hospital may do things slightly differently, and treatment will vary depending on your cancer. Speak to your doctor or nurse about your treatment.
Each hospital may do things slightly differently, and treatment will vary depending on your cancer. Speak to your doctor or nurse about your treatment.
FOLFIRINOX is made up of a combination of chemotherapy drugs:
• FOL – folinic acid (leucovorin), which is a vitamin that helps fluorouracil work better
• F – fluorouracil (5FU)
• IRIN – irinotecan
• OX – oxaliplatin.
Sometimes folinic acid, 5FU and oxaliplatin are used without irinotecan. This is known as FOLFOX. Read more about FOLFOX.
Sometimes folinic acid, 5FU and irinotecan may be used without oxaliplatin. This is known as FOLFIRI.
FOLFIRI may be used for people who are having problems with side effects of oxaliplatin, such as tingling and numbness in their hands and feet (peripheral neuropathy). It may also be used as a second-line treatment for people who have already had a gemcitabine based chemotherapy.
FOLFIRI is given in the same way as FOLFIRINOX, but without the oxaliplatin.
Your chemotherapy team can talk to you about these options.
FOLFIRINOX is used in different ways:
This treatment is only given to people who are well enough for a few different chemotherapy drugs. This is because FOLFIRINOX can cause side effects that can be hard to deal with.
You will have your chemotherapy at the hospital as an outpatient. This means that you will go into hospital for treatment, but you won’t need to stay overnight.
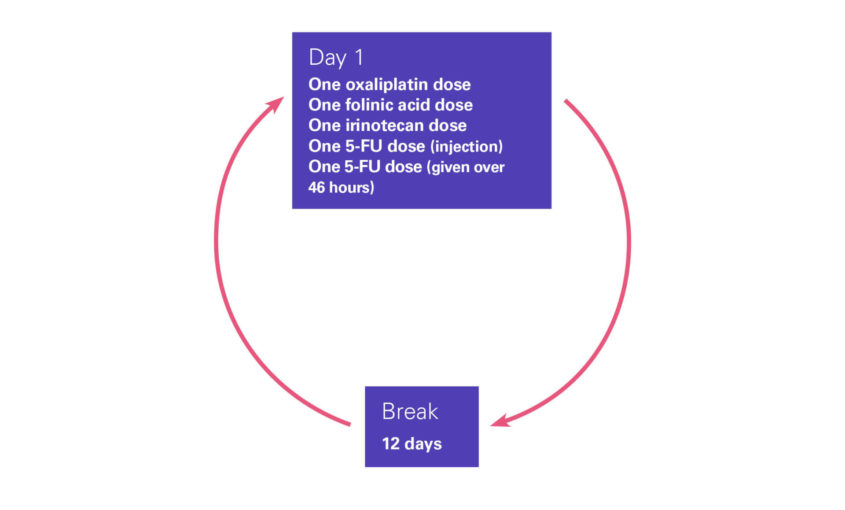
FOLFIRINOX is given in a two-week cycle. This means you will have the chemotherapy over two days, and then a break of 12 days before you have the next cycle. The break allows your body to recover. The number of cycles you have will depend on how the treatment is working and how chemotherapy affects you. Your chemotherapy team will talk to you about your treatment cycles.
The FOLFIRINOX drugs are given as an injection or infusion into a vein. You may hear an infusion called a ‘drip’. You will have the infusion through a cannula, or through a central line – such as a PICC line or a portacath. The line will be flushed out between each different drug.
On the first day of each cycle, you will have an infusion of oxaliplatin, folinic acid and irinotecan. You will then have an injection of fluourouracil into a vein. This will all take about six hours, but check this with your chemotherapy team, as it may vary at different hospitals. After this you will have an infusion of fluourouracil over 46 hours. This is given through a small pump attached to your central line. You can have this at home by attaching the pump to a belt and carrying it around with you. You will then have a break from chemotherapy for the next 12 days.
Each chemotherapy team may give FOLFIRINOX slightly differently. For example, you may have oxaliplatin and folinic acid one after the other, or you may have them at the same time. Speak to your chemotherapy team about how you will be given FOLFIRINOX.
Diagram showing how FOLFIRINOX is given
Some people may have a reaction while FOLFIRINOX is being given.
Signs of a reaction are:
Some people may also have runny poo (diarrhoea) or tummy pain, caused by a reaction to the infusion.
These reactions need treating straight away, so if you have any of these symptoms or anything else unusual, tell the nurse giving you chemotherapy.
FOLFIRINOX can cause side effects, but these can affect everyone differently, and you may not get all the side effects mentioned here. Your chemotherapy team should give you information about any possible side effects and how to manage them. They may give you medicines to help with side effects to take home and use when you need to. Ask the team any questions you have. Knowing what to expect can help you to cope with any side effects.
If you have lots of side effects, your doctor may change the dose of some of the FOLFIRINOX drugs to make it easier to cope with. This is sometimes known as mFOLFIRINOX (modified FOLFIRINOX). Your chemotherapy team can talk to you about this.
Fluorouracil (5FU) is broken down in the body by an enzyme called dihydropyrimidine dehydrogenase (DPD). Some people have lower amounts of the DPD enzyme, which is known as DPD-deficiency. People with DPD-deficiency can have side effects that are much worse than usual. These include infections, runny poo (diarrhoea) and feeling or being sick. You will have a blood test to check for DPD-deficiency before you start chemotherapy.
Your chemotherapy team should give you a 24 hour emergency number to call if you are unwell, have any signs of infection, or if you need information about any side effects. Your nurse will explain when to use this number. If you haven’t been given a number, ask your nurse about this.
FOLFIRINOX can increase your risk of getting an infection. An infection is an emergency if you are having chemotherapy, and needs treating straight away. Signs of an infection include:
Call the 24 hour emergency number your chemotherapy team will have given you if you have signs of an infection. You should phone if you have any of these symptoms or feel suddenly unwell, even if your temperature is normal or low.
Read more about infections and how they are treated.
If you have diarrhoea, try to drink as much water as you can. If you are finding it hard to drink enough fluids, contact your chemotherapy team. If you have diarrhoea more than four times a day, tell your chemotherapy team. They can give you medicines to control it. Your chemotherapy may be delayed until the diarrhoea is better, or the dose of your chemotherapy drugs may be lowered.
Read more about diarrhoea and how it is treated.
Constipation is when you find it harder to poo. Drink as much water as you can manage and try to eat high fibre foods, such as fruit and vegetables. Gentle exercise such as walking can also help. Speak to your doctor about medicines that can help.
Fatigue is a common side effect of FOLFIRINOX. It is not the same as feeling tired. Fatigue can make you feel weak and have problems concentrating. Some people find that the fatigue starts a few hours to a few days after having chemotherapy and starts to get better after a few days. There are things that you can do to help with fatigue. Read our tips on coping with fatigue.
Oxaliplatin may also cause dizziness. Feeling tired and dizzy can affect your ability to drive. You might want to get someone else to drive you until you know if you are affected.
This is a common side effect of FOLFIRINOXbut you can take medicines to stop you feeling or being sick. You will normally be given anti-sickness medicines to manage sickness. If these medicines don’t help, speak to your chemotherapy team about changing to a different medicine.
Read more about feeling and being sick, and some tips for coping with it.
FOLFIRINOX can affect the nerves in your hands and feet, which can cause tingling and numbness. This is called peripheral neuropathy. It normally gets better after your treatment finishes, but for some people it may never go away. This can be worse in the cold, so wrap up well if you are going outside.
Talk to your chemotherapy team if you have any tingling or numbness in your fingers or toes. Read more about peripheral neuropathy and how it is managed.
Oxaliplatin can affect your throat, which can make it hard to swallow or breathe. If this happens when you are being given oxaliplatin, tell your nurse straight away. They may stop the infusion of oxaliplatin while they give you medicine to help with this.
You may also get this side effect in the first few hours after having oxaliplatin, but this is normally only if you are out in the cold or having a cold drink. It should stop a few days after your treatment finishes. Try to avoid cold drinks and wrap up warmly if you go out in the cold.
FOLFIRINOX can lower the number of red blood cells in your blood. This is called anaemia, and can make you feel tired, dizzy or short of breath. If any of these symptoms happen suddenly, call the emergency number. If your red blood cell level is very low, you may need to be given blood through a drip. This is called a blood transfusion. Read more about anaemia.
FOLFIRINOX can lower the number of platelets in your blood. This is called thrombocytopenia. You may bruise more easily than normal, and you may be more likely to have nosebleeds or bleeding gums. If you have a nosebleed that does not stop after five minutes, call the emergency number.
FOLFIRINOX may cause your hair to thin, or you may lose some hair – but it should grow back once your treatment stops. Read more about chemotherapy and hair loss.
FOLFIRINOX may cause a funny taste in your mouth. Some people say this tastes like metal or cardboard. You may find that food loses its flavour, or you stop enjoying some foods or drinks. This normally gets better once you finish your chemotherapy. You might find our tips for coping with taste changes helpful.
During your treatment you may not feel like eating, and you may start to lose weight. Try eating small meals often. If your appetite doesn’t get better after a few days, tell your doctor or dietitian. We have tips on dealing with a loss of appetite.
FOLFIRINOX can make your mouth sore, or cause mouth ulcers which can be painful. Tell your chemotherapy team about any problems you have with your mouth. They can make sure you don’t have a mouth infection and give you a mouthwash which should help. You should also tell them if you have white spots in your mouth. This is a sign of oral thrush, which is normally easy to treat.
FOLFIRINOX can make the palms of your hands and the soles of your feet red and sore. The skin may also start to peel. Your doctor or nurse may give you a vitamin or creams to help with this. If you have badly peeling skin, it is very painful, or you have broken skin that looks infected, call the emergency number. The soreness normally gets better when your chemotherapy finishes.
Oxaliplatin can cause problems with your joints, such as swelling or pain. Let your doctor or nurse know if you have this side effect. They can give you painkillers to help. Make sure that you check your temperature before taking any paracetamol or ibuprofen. If you have a high temperature, call the emergency number straight away.
FOLFIRINOX can make your skin darken or become more sensitive to the sun. Use a high factor sun cream if you are going outside. Tell your chemotherapy team about any skin changes. These changes normally get better when your treatment finishes.
FOLFIRINOX can cause sore, itchy or watery eyes. Tell your doctor or nurse if this happens, as they may need to give you some eye drops. Some people get blurred vision when having FOLFIRINOX, but this is less common.
Fluorouracil can cause chest pain. It can also make you feel short of breath, dizzy, or cause an irregular heartbeat. It is important to tell your chemotherapy team straight away if you have any of these symptoms. If you have chest pain, go straight to A&E and tell them you are having chemotherapy.
Chemotherapy can increase the risk of a blood clot in a vein. If you have any pain or swelling in one of your arms or legs, or you feel short of breath, call the emergency number straight away. Or phone an ambulance and tell them you are having chemotherapy. A blood clot is serious if it’s not treated.
Speak to your chemotherapy team if you experience anything unusual, or if you would like more information.
You can also speak to our specialist nurses on our free Support Line.

You can download our fact sheet on FOLFIRINOX for pancreatic cancer.
Updated April 2022
Review date April 2024